Optimising chronic oedema patient treatment
This information provides help for healthcare professionals to safely guide, educate and optimise chronic oedema and lymphoedema in partnership with patients – reducing the burden on patients and community nurses.
What is chronic oedema and lymphoedema?
‘Chronic Oedema’ is used interchangeably with the term ‘Lymphoedema’. It is a term used to describe a group of conditions characterised by the presence of swelling within tissues of the body, caused by the accumulation of excess fluid within the interstitial space of the affected area.
Oedema most commonly affects the lower or upper limbs, but may also affect midline structures such as the head and neck, trunk, breasts or genitalia. Oedema results from an imbalance between capillary filtration into and lymphatic drainage from tissue space.
Although the term ‘lymphoedema’ suggests that the oedema is caused by a lymphatic abnormality, in every case of chronic oedema there will be some impairment of lymphatic drainage, either through an underlying abnormality (‘primary’ or ‘secondary’) or through ‘lymphatic failure’ as a result of the lymphatics being overloaded. The degree to which the lymphatics are, or become affected may influence the clinical presentation of the oedema, the tissues and skin.
What does chronic oedema look like?
Here’s an example of chronic oedema with skin folds, skin changes and unmanaged oedema.

DOWNLOAD: LYMPHOEDEMA THE FACTS
Levels and types of oedema
Not all cases of oedema are chronic / lymphoedema – there are also mild and moderate cases.
Early intervention is crucial. Do not ignore and think it will resolve as the likelihood is, it will potentially deteriorate and move towards chronic oedema, causing distress and a requirement for longer treatment. Do not regard it as something that happens as a result of age, medication or lifestyle.
Mild oedema of the feet

Moderate oedema to left leg

What is cellulitis or red legs?
Cellulitis is a dangerous infection, red legs can indicate a variety of symptoms. It is vital to know the difference and neither can be ignored.
If you suspect cellulitis, the affected area should be marked and immediate treatment sought from a GP. Treatment is with antibiotics and hospital admission is sometimes necessary.
What does chronic cellulitis look like?

Cellulitis episodes are common prior to diagnosis of chronic oedema / lymphoedema and should be a red flag to indicate the condition/s.
The treatment may differ from conventional cellulitis in that it may be required for a longer period as well as effective management in compression. Maintenance post treatment is required to prevent recurrence.
DOwnload: BLS’ CONSENSUS DOCUMENT
What is lymphorrhoea (wet leaky legs)?
Lymphorrhoea is the flow or discharge of lymph fluid through the skin. This leaking will occur when oedema is untreated as the swelling will increase, therefore not allowing the skin to manage or accommodate the fluid.
It appears as beads of fluid which put the affected area at risk of skin damage since the skin becomes very wet and broken and the likelihood of cellulitis is also increased.
What does lymphorrhoea look like?
DOWNLOAD: LYMPHORRHOEA IN THE COMMUNITY
Assessment of oedema / swelling
Robust assessment is vital in ensuring a correct diagnosis, understanding the underlying cause and to determine collaborative next steps to positive patient outcomes. During Covid-19, patients may have become less mobile and less conscientious in their care, potentially increasing the risk of oedema becoming chronic.
There are important steps to assessment:
Establish the cause
- Explore the story and medical history behind the swelling
- Are there any underlying conditions?
- When did it start – was it sudden or gradual, unilateral or bilateral?
- Is there a history of repeated cellulitis infection?
- What may be impacting the cause e.g. not getting to bed, decreased mobility, obesity?
Examine the limb(s)
- Feel the tissues
- Are the tissues pitting or fibroses?
- What skin changes are noted
- Take careful note of the size and shape of the limb to ensure progress / deterioration can be measured
- The size of the limb should be evaluated at initial assessment to obtain a baseline set of measurements to refer to throughout the patient’s journey to chart their progress.
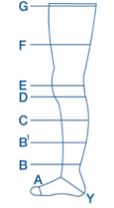
Simple measurements taken from set points above the malleolus, mid-calf and at mid-thigh can be enough to assess progress with treatment. Measuring and recognising the shape of the limb will determine treatment choices and if further signposting or referral is needed.
Understand your patient
- Their ability and willingness to self manage
- What key areas are achievable to self-manage
- Their priorities
- Explore any areas of concern which need to be built upon
This video shows how to encourage your patient to begin to gain a better understanding of their condition and how to have better conversations.
Set goals
- Realistic and jointly agree the plan
- Take a step wise approach
For further support in assessment please see the attached collaborated consensus document kindly provided by BSN Medical.
DOWNLOAD: ASSESSMENT OF OEDEMA
Treatment
Ensure treatment is tailored to the individual’s needs as a ‘one fit for all’ approach may result in longer, unnecessary treatment for the patient.
Jointly agree the holistic treatment plan and ensure the patient is fully informed of next steps to aim for continued improvement and maintenance of the swelling.
The three main components of a treatment plan must include the following:
- Skin care
- Compression therapy
- Exercise
Skin care
Ensuring a daily, simple skin routine can maintain the integrity of the skin whilst preventing and reducing the risk of infection such as cellulitis.
Three simple steps:
- Cleansing
- Drying
- Moisturising
Make sure you include the full affected limb, between the toes or any other crevasses to optimise treatment and allow a thorough inspection of the limb for both professional and patient.
If a wound is present, ensure the wound is also cleansed to again optimise healing. Please see the below video link on how to undertake robust skin care:
WATCH: Susceptibility to cellulitis FILM
Compression
Compression therapy is the main vital component in limb volume reduction and long term management. This may take the form of bandaging, hosiery or wraps. During Covid-19 more than ever, ensuring compression is working, comfortable and fit for purpose is vital and promotes a positive patient experience and outcomes.
What to consider when selecting compression treatment:
- Garment type
- Size & shape of limb
- Patient preference / tolerance linked to lifestyle
- Patient ability to self manage
- Frequency of visits / treatment needed
- Clinician expertise
- Presence of a wound
Guides for how to apply compression hosiery
There are a variety of products available – if you cannot see what you need here please contact Accelerate for further support.
Here’s a video with demonstration of different donning and doffing aids for compression hosiery.
Watch: LYMPHOEDEMA AND COMPRESSION GARMENTS
Guides for how to apply compression wraps
Again, there are a variety of products available – if you cannot see what you need here please contact Accelerate for further support.
Training is available for different bandage techniques for patients with chronic oedema, lymphoedema, lymphorrhea and wet toes by contacting Accelerate directly or viewing what’s on offer on Accelerate Academy.
Application and removal of ReadyWrap compression garment.
Exercise
It is imperative that patients with oedema and lymphoedema partake in regular daily exercise to minimise an increase in their BMI whilst addressing their overall wellness.
The aim is to promote a healthy drainage, minimise its effects and to help slow the progression of the condition.
An exercise programme should include the following:
- Stretching – to increase the range of motion at joints that are tight
- Strengthening – to improve muscle performance and strength
- Endurance – to improve the efficiency of the heart, lungs, and muscles
If you are looking for specific exercises suitable for patients with leg or arm swelling here’s a series of useful videos.
VIDEO – Leg exerciseS for Lymphoedema
VIDEO – Arm exercises for lymphoedema
VIDEO – Exercises with a TheraBand
Encourage your patients to try some simple exercises, they are often surprised at the results. Keeping an exercise record is really helpful.
PDF – EXERCISE RECORD FOR LYMPHOEDEMA PATIENTS
Simple lymphatic drainage
Lymphatic drainage is a specialised, gentle type of medical massage which helps control swelling. The aim is to encourage the lymph fluid to move away from the swollen area so it can drain normally. It also helps lymph fluid drain through the healthy lymph vessels.
There are two main types of lymphatic drainage:
- Manual lymphatic drainage (MLD)
- Simple lymphatic drainage (SLD)
You should only have MLD from a trained lymphatic drainage therapist, it is a short course of treatment. SLD is something which patients can undertake themselves.
You should not use other types of massage on the affected area.
If you identify patients who may benefit from learning SLD, please contact Accelerate on 020 8138 4857.
Thanks to The BLS for allowing us to share their content.